Errors Due to the Presentation of Results on Accu-Chek Inform II and Possibly Other Glucometers
Problem: Glucose testing is one of the most frequent point-of-care (POC) tests performed in hospitals.1 While POC glucose testing offers immediate results that can be used to make important clinical decisions about the treatment of hypo- or hyperglycemia, errors can occur at any point in the testing process. For example, earlier studies have found that the most common types of errors associated with POC glucose testing are related to delays in testing due to the unavailability of trained staff2 and a failure to positively identify patients prior to testing.3 In the latter case, a study in a neonatal unit showed that staff failed to confirm two patient identifiers for 45% of the POC tests performed.3 Other factors that can affect POC glucose test results include hematocrit, ascorbic acid levels,4 and other sugars such as maltose,5 including maltose-containing medications or parenteral solutions.6,7
VHA Study
In a more recent study conducted by the Veterans Health Administration (VHA),8 a different type of error was described. The study was conducted in response to multiple adverse events reported to the US Food and Drug Administration (FDA) since 2010. These events involved mistakes in interpreting patients’ blood glucose levels due to the way the results were displayed on some glucometer screens, including ACCU-CHEK Inform (no longer available from the manufacturer) and ACCU-CHEK Inform II (Roche Diagnostics), a commonly used POC glucometer by the VHA. In the events reported to FDA, practitioners misinterpreted the results on the glucometers when the blood glucose was displayed using an out-of-range abbreviation, such as RR LO (out of reportable range; low limit) or CR LO (out of critical range; low limit), and/or when numeric alarm codes (e.g., W-510) were displayed in a pop-up message. One error occurred when CR LO was misinterpreted as a high blood glucose reading, and insulin was incorrectly administered to the patient.9 Two other events occurring within 3 months of each other involved the abbreviation RR LO, which was also misinterpreted as a high blood glucose reading.10,11 Insulin was incorrectly administered to both patients, one of whom died. In the fatal event, the practitioner expected a numeric blood sugar value to appear on the results screen, so the numeric portion of the alarm code, W-510 (Figure 1), was presumed to be the patient’s blood glucose value.11

The Accu-Chek Inform II can display critical blood glucose levels 6 different ways depending on glucometer configuration. For example, for a blood glucose value of 32 mg/dL, 4 of the 6 configurations will display an out-of-range abbreviation (CR LO or RR LO)—2 of which will include a numeric alarm code. Figure 1 provides an example of 1 of these 4 configurations, RR LO with alarm code W-510. Two of the 6 configurations will display a numeric blood glucose value (e.g., 32 mg/dL), 1 of which will include a numeric alarm code. Figure 2 provides an example of 1 of these 2 configurations with alarm code W-511. Thus, the VHA conducted a study to determine the safest way to configure the Accu-Chek Inform II glucometers that would lead to the fewest treatment errors.8
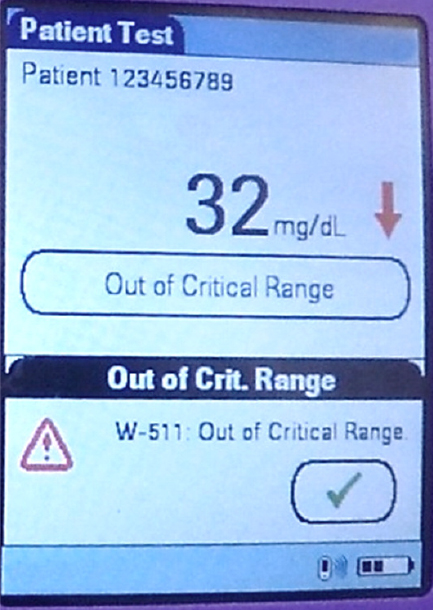
The 6 different ways of displaying blood glucose results were first evaluated against 7 usability principles related to language, expectations, error codes, memory load, word meanings, terminology, and abbreviations. All configurations violated at least 1 usability principle. However, it was expected that displaying a low blood glucose value as RR LO, with a numeric alarm code (Figure 1), would result in the most treatment errors given that it violated all 7 usability principles, and that displaying a blood glucose as a numeric value, with a numeric alarm code (Figure 2) would result in fewer treatment errors, as it violated only 3 usability principles. Thus, these 2 configurations were tested.
Using a computer-based simulation at two different Veterans Affairs (VA) medical centers, a total of 66 registered nurses (86%) and licensed practical nurses (14%), who were trained and experienced with using the Accu-Chek Inform II, were provided with clinical scenarios of hospitalized patients with diabetes. For each scenario, blood glucose values were displayed in 2 different configurations. The nurses were then asked how they would interpret these results and treat the simulated patients based on their interpretation of the results displayed on the glucometer. Although technicians and nursing assistants are also common users of the glucometers, they were not included as participants in the study because interpretation of the results and treatment decisions were outside their scope of practice. Most of the participating nurses used the Accu-Chek Inform II glucometers daily, although only half of the nurses received prior education regarding the meaning of RR LO.
Study Results
When testing for treatment decision errors, 1 in 10 nurses misunderstood the abbreviation RR LO and did not choose to administer juice or 50% dextrose to the simulated hypoglycemic patient per policy. In fact, almost half of the nurses who misinterpreted the RR LO abbreviation chose to administer additional insulin to the simulated patient. Furthermore, some of the nurses (6.7%) who had prior training and exposure to the RR LO reading made a treatment decision error, misinterpreting the correct meaning of the abbreviation. None of the nurses made a treatment decision mistake when the glucometer displayed the numeric blood glucose value (32 mg/dL) instead of the abbreviation.
When evaluating interpretation of the results displayed on the screen, 6-7% of all participants made an error with either configuration. However, most of the nurses who made errors when interpreting the numeric blood glucose value of 32 mg/dL recognized that the value was low and made the correct treatment decision but did not think the value was critically low. According to a knowledge survey conducted with the study, 99% of all participants knew that 32 mg/dL was a critically low blood glucose; however, the message “Out of Critical Range” could have been misinterpreted as a message that the value was not critically low. Most of the nurses who misinterpreted the RR LO abbreviation decided that it was a critically high blood glucose value because they misinterpreted the pop-up message “W-510” as a high blood sugar value. For participants who correctly interpreted both configurations, more than three-quarters required more time to interpret an RR LO reading than a 32 mg/dL reading.
The results confirmed that displaying a numeric blood glucose reading eliminated potentially life-threatening treatment errors caused by confusing abbreviations. The results also suggest that prior training can help but cannot eliminate the risk of errors when out-of-range abbreviations are displayed. The study also showed that nurses were faster at interpreting numeric blood glucose readings compared to out-of-range abbreviations, which can help facilitate rapid treatment decisions for patients experiencing critically high or low blood glucose levels.8 Although not tested during the study, mistakes are also possible when the abbreviations RR HI (out of reportable range; high limit) and CR HI (out of critical range; high limit) appear on the glucometer.
Safe Practice Recommendations: To avoid misinterpretation of blood glucose results on POC testing glucometers and incorrect treatment decisions, consider the following recommendations:
If you use Accu-Chek Inform II glucometers
- Set the reportable range to match the entire measurement range of the device (10 mg/dL to 600 mg/dL) to prevent the display of RR LO or RR HI abbreviations.8
- Configure the critical results to display as a numeric value to prevent the display of CR LO or CR HI abbreviations.8 (This setting and the one above match the default configurations documented by the manufacturer.)
- During educational programs and simulation training, include a description of out-of-range abbreviations, obscure alarm codes, and alert language that may appear on the results screen, their intended meaning, and the risk of confusion.
If you use another type of glucometer
- Evaluate the display of blood glucose results on glucometers used in the facility to determine if it contains potentially confusing language, terminology, alarm codes, or abbreviations. Whenever possible, configure glucometers to display the actual numeric blood glucose value rather than out-of-range codes and confusing alarm messages. Contact the manufacturer if necessary, or consider changing to a different manufacturer’s glucometer that allows such a configuration. Alert staff to the meaning of any alarm codes and warning messages if they must be displayed on the screen, particularly if they include numeric values.
Manufacturers and FDA
- Strongly consider the findings from this study during future research and development of POC glucometers. Confusing language, obscure alarm codes that appear on results screens, unexpected presentation of blood glucose results as out-of-range abbreviations rather than numeric values, overreliance on memory regarding numeric ranges associated with the abbreviations, and other heuristics associated with usability and effectiveness of the glucometers in guiding treatment decisions should be addressed with future upgrades to the technology.
References
- Shaw JLV. Practical challenges related to point of care testing. Pract Lab Med. 2016;4(1):22–9.
- O’Kane MJ, McManus P, McGowan N, Lynch PL. Quality error rates in point-of-care testing. Clin Chem. 2011;57(9):1267-71.
- Cantero M, Redondo M, Martin E, Callejón G, Hortas ML. Use of quality indicators to compare point-of-care testing errors in a neonatal unit and errors in a STAT central laboratory. Clin Chem Lab Med. 2015;53(2):239-47.
- Heinemann L. Quality of glucose measurement with blood glucose meters at the point-of-care: relevance of interfering factors. Diabetes Technol Ther. 2010;12(11):847-57.
- Schleis TG. Interference of maltose, icodextrin, galactose, or xylose with some blood glucose monitoring systems. Pharmacotherapy. 2007;27(9):1313-21.
- ISMP. FDA Advise-ERR. Prevent dangerous drug-device interaction causing falsely elevated glucose levels. ISMP Medication Safety Alert! 2008;13(12):1-3.
- ISMP. Be aware of false glucose results with point-of-care testing. ISMP Medication Safety Alert! 2005;10(18):1-3.
- Estock JL, Pham IT, Curinga HK, et al. Reducing treatment errors through point-of-care glucometer configuration. Jt Comm J Qual Patient Saf. 2018;000:1-12.
- FDA. MAUDE adverse event report: Roche Diagnostics Accu-Chek Inform meter blood glucose monitoring device. April 29, 2010.
- FDA. MAUDE adverse event report: Roche Diagnostics Accu-Chek Inform II test strips blood glucose monitoring test strips. November 3, 2015.
- FDA. MAUDE adverse event report: Roche Diagnostics Accu-Chek Inform meter blood glucose monitoring device. January 17, 2016.
